- About us
- A new Institute dedicated to combating leukemia
- Scientific and medical program
- History of Hematology on the Saint-Louis Campus
- The Leukemia Institute’s governance
- Press
- Contact us
- Our news
- Profile of Valéria Bisio, Research Officer
- Creation of a Hemato-Oncogenetics Unit
- Profile of Alice Gros, a peer-support patient
- Winners of the Leukemia Institute’s first call for projects
- Profile of Julien Calvo, researcher
- Support us
- Join us
- You are
- Patients and relatives
- To receive care and support
- Become an expert patient
- Discover the Leukemia Institute
- Researchers
- Research
- Clinical trials
- Discover the Leukemia Institute
- Healthcare professionals
- Refer a patient
- Our clinical research
- Discover the Leukemia Institute
- Industry partners
- Discover the Leukemia Institute
- Translational research
- Donors
- Support us
- Discover the Leukemia Institute
- Care
- Patient care
- Being Treated at the Leukemia Institute
- Cancer treatments
- Supportive Care
- Open Multidisciplinary Meetings
- Our clinical services
- Saint-Louis Hospital – Department of adult hematology
- Saint-Louis Hospital – Hematology Transplant Unit
- Saint-Louis Hospital – Department of Pharmacology and Clinical Investigations
- Saint-Louis Hospital – Adolescent and Young Adult Unit
- Saint-Louis Hospital – Outpatient Hemato-oncogenetics Unit
- Saint-Louis Hospital – Department of senior hematology
- Robert-Debré Hospital – Department of pediatric hematology and immunology
- Necker Hospital – Department of Adult Hematology
- Cochin–Port Royal Hospital – Department of clinical hematology
- Avicenne Hospital – Department of clinical hematology and cell therapy
- Our medical laboratories
- Hematology Medical Laboratory, Michaela Fontenay
- Hematology Medical Laboratory, Jean Soulier
- Molecular Genetics Unit, Hélène Cavé
- Hematology Medical Laboratory, Vahid Asnafi
- Patient information
- Acute Myeloid Leukemias
- Acute Lymphoblastic Leukemias
- Myeloproliferative Neoplasms
- Myelodysplastic Syndrome
- Cancer treatments
- Supportive Care
- Psychological Support
- Research
- Our research teams
- Hugues de Thé’s team – Molecular pathology
- Raphaël Itzykson’s team – Functional precision medicine for leukemia
- Michaela Fontenay’s team – Normal and pathological hematopoiesis
- Françoise Pflumio’s team – Niche, Cancer, and Radiation in Hematopoiesis
- Sylvie Méléard’s team – Population Evolution and Interaction Particle Systems
- David Michonneau’s team – Translational Immunology in Immunotherapy and Hematology (TIGITH)
- Lina Benajiba’s team – Identification and targeting of extrinsic regulators of myeloid malignancies
- Karl Balabanian’s team – Lymphoid niches, Chemokines and Immuno-hematological syndromes
- Alexandre Puissant’s team – Molecular Mechanisms of Acute Myeloid Leukemia Development
- Stéphane Giraudier’s team – Chronic Myeloid Malignancies, Microenvironment & Translational Research
- Diana Passaro’s team – Leukemia & Niche Dynamics
- Camille Lobry’s team – Genetic and Epigenetic control of Normal and Malignant Hematopoiesis
- Jean Soulier’s team – Stem cell dysfunction and secondary AML
- Sylvie Chevret’s team – Biostatistics and clinical epidemiology
- Our technological platforms
- Our clinical research
Accueil Lina Benajiba’s team – Identification and targeting of extrinsic regulators of myeloid malignanciesLina Benajiba’s team – Identification and targeting of extrinsic regulators of myeloid malignancies
...Lina Benajiba
Team leader
Institut de recherche Saint-Louis
Research themes
Although oncogenic driver mutations are found in healthy tissues, they do not often result in overt cancer.
This genotype – phenotype discrepancy warrens the search for extrinsic mechanisms of cancer development and maintenance, such as exposition to specific environments. Using myeloid neoplasms as a cancer model, our multidisciplinary team aims at dissecting the hematopoietic-niche partnership to identify innovative therapeutic strategies to prevent acute myeloid leukemia development, maintenance and recurrence.
- Myeloproliferative neoplasms
- Acute myeloid leukemia (AML)
Research areas
Leukemic transformation is a complex process that could result from the life-long therapeutic intervention needed to treat MPN chronic phase, and/or from microenvironment-related signals.
To decipher the mechanism of pre-leukemic to leukemic state transition, the team develops a comprehensive translational approach combining data mining of an extensively annotated database, in vitro and in vivo models and large-scale functional and descriptive genomic approaches.
We aim at highlighting potential therapy related selection of highly detrimental mutations and deciphering its underlying mechanisms. We are also interested in the effects of MPN treatments on non-hematopoietic organs, particularly the skin. In parallel, we aim at discovering and validating novel niche-hematopoietic crosstalk transformation promoting pathways.
Our discoveries should contribute to better understanding environmentally induced MPN clonal evolution, offering a path towards therapeutically preventing leukemic transformation.
The bone marrow niche plays a key role in sustaining AML and regulating drug resistance.
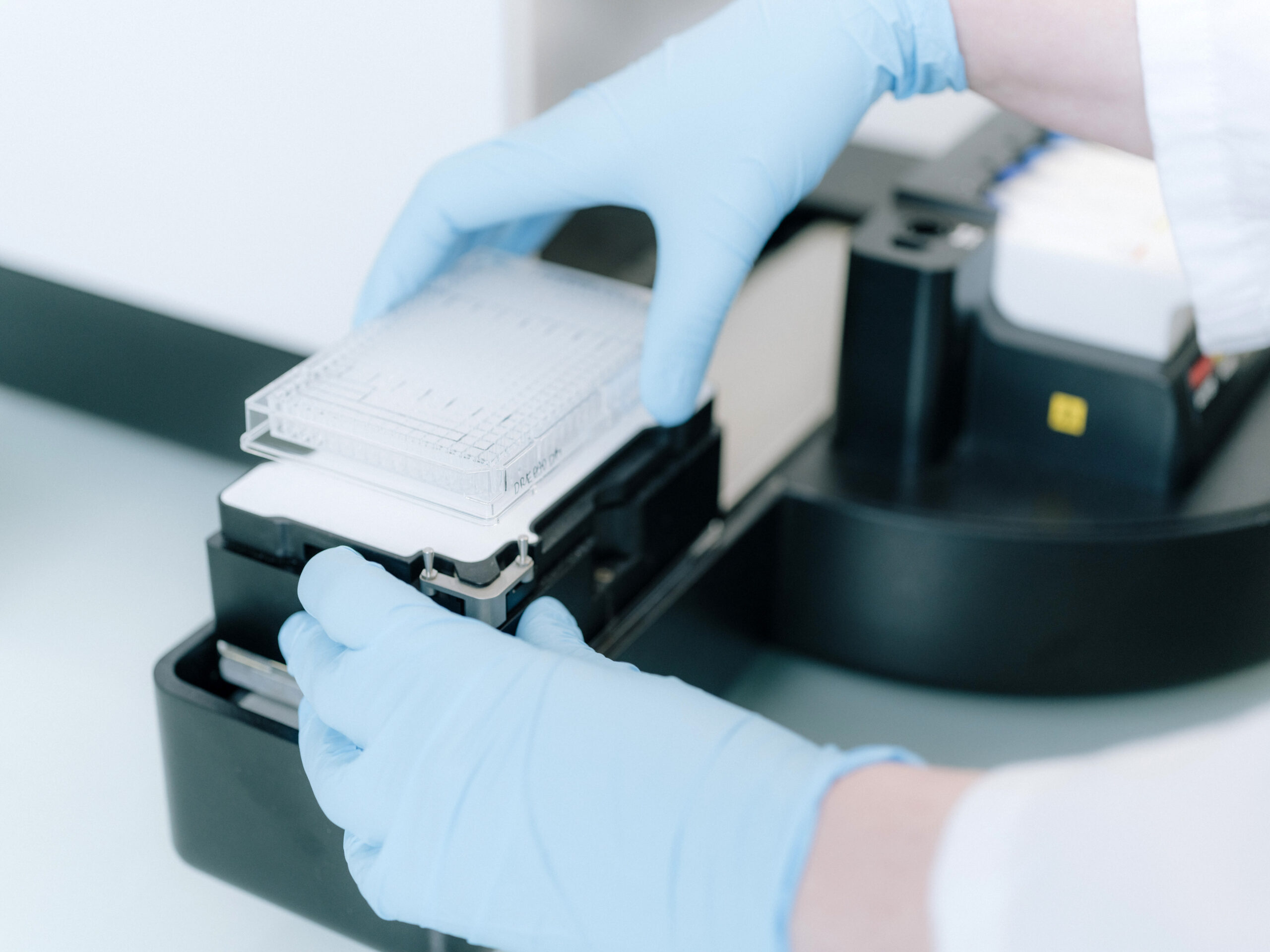
Our goal is to define novel niche-leukemic crosstalk induced dependencies, through combining single-cell omic approaches to high-throughput screening tools applied to custom-made in vitro and in vivo models.
Our team develops humanized mouse models, closely mimicking the physio-pathological conditions of leukemic cells growth within the bone marrow microenvironment.
In collaboration with Saint-Louis hospital clinical departments, we develop a pipeline to identify innovative therapeutic targets and conduct the necessary preclinical steps towards translating our findings to the clinic, including identification of response biomarkers and synergy studies.
In parallel, we are highly interested in shedding light on the mechanistic underpinnings of the bone marrow-leukemia crosstalk.
Our findings should open the road for concomitant “seed” and “soil” targeting strategies, resulting in AML leukemic stem cells eradication and patient’s survival improvement.
Patients with AML are at higher risk of early death due to severe infectious complications (sepsis), tissue infiltration by blast cells, leukostasis or tumor lysis syndrome.
Our team investigates the pathophysiological mechanisms underlying these life-threatening complications and their subsequent acute organ failure.
Using in vitro and in vivo models, we focus on endothelial dysfunction’s key role.
In parallel, we are highly interested in how essential cellular and molecular signals triggered by sepsis-induced inflammation alter the bone marrow microenvironment and influence leukemic cells proliferation and AML progression.
Our work aims to uncover novel therapeutic strategies to improve patient survival by mitigating acute AML-associated complications and their potential long-term impact on disease evolution.
Featured research projects
VCP as a Novel Therapeutic Target in AML
AML cells are dependent on the DNA repair function of the AAA-ATPase VCP, opening up a therapeutic avenue with a newly developed second-generation VCP inhibitor, CB-5339
Blandine Roux
Therapy-induced clonal selection of RAS pathway mutations in myeloproliferative neoplasms
JAK inhibitors promote clonal selection of RAS mutations, resulting in increased oncogenic potential and impacting patients overall and transformation free survivals
Nina Kaci
JAK inhibition intrinsic and extrinsic effects in skin cancer
JAK inhibition results in increased risk of skin cancer through MAPK pathway activation, while positively remodelling the tumor immune microenvironment to create new therapeutic avenues in combination with immune checkpoint inhibitors
Hélène Pasquer
Lina Benajiba's team members
Lina BENAJIBAMD,PhD, HDR – Associate Professor (MCU-PH) – Team LeaderLara ZafraniMD, PhD, HDR – Full professor (PU-PH) – Principal InvestigatorHélène PasquerMD, PhD – Assistant Professor (CCA-INSERM-Bettencourt)Stéphanie PONSMD, PhD – PHC – Principal InvestigatorEmmanuel RaffouxMD –Associated Professor – Associated ClinicianFlorence RabianMD – PH – Associated ClinicianCécile CuleuxLab managerLéa ProventResearch AssistantMorgane DenisPhD, Postdoctoral fellowAlexandre FagnanPhD, Postdoctoral fellowAurélie ClaquinPhD StudentFederica NamorPhD StudentNabila SakerPhD StudentScientific publications
Blandine Roux & al, Sci Transl Med, 2021
Targeting acute myeloid leukemia dependency on VCP-mediated DNA repair through a selective second-generation small-molecule inhibitorRead the publicationKhansa Saadallah & al, EMBO reports, 2025
AML patient blasts exhibit polarization defects upon interaction with bone marrow stromal cells.Read the publicationNabih Maslah & al, Nature Communications, 2025
JAK2 inhibition mediates clonal selection of RAS pathway mutations in myeloproliferative neoplasmsRead the publicationJoin us
Please get in touch if you are interested in joining the team at all levels.
Our lab is always eager to welcome passionate young scientists.
You can contact us at the following address: lina.benajiba@inserm.fr
Stay up to date by subscribing to the institute's newsletter
- Discover the Leukemia Institute
- Translational research
- Our clinical research
- Clinical trials
- Become an expert patient
- To receive care and support
- A new Institute dedicated to combating leukemia